The new coronavirus can infect brain cells, according to studies
The coronavirus that causes COVID-19 can in some cases hijack brain cells, utilizing the cells’ internal machinery to copy itself, as indicated by another study.
The research, posted Sept. 8 to the preprint database bioRxiv, has not yet been distributed in a companion looked into journal, however it gives proof that SARS-CoV-2 can straightforwardly infect brain cells called neurons.
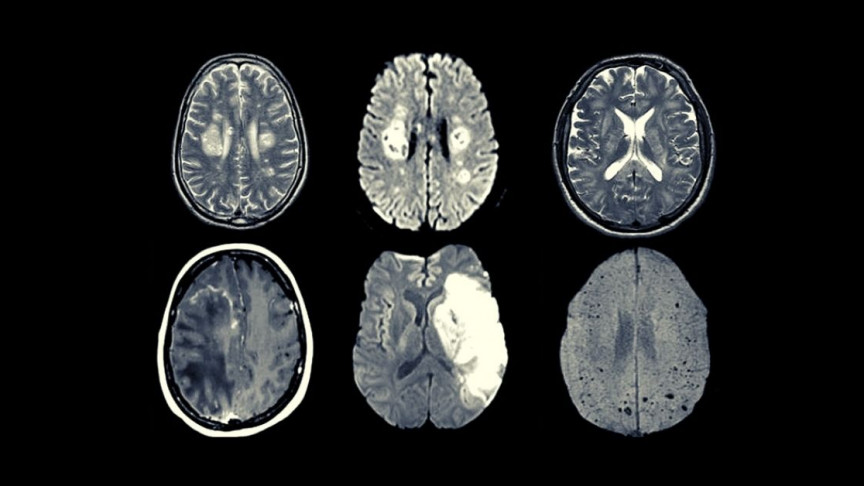
Despite the fact that the coronavirus has been connected to different types of brain harm, from dangerous irritation to brain sicknesses known as encephalopathies, all of which can create turmoil, mind haze and incoherence, there was little proof of the infection itself attacking cerebrum tissue as of not long ago.
“We are actively looking at more patient tissues to be able to find how frequently such brain infections occur … and what symptoms correlate with infection of which areas of the brain,” senior creator Akiko Iwasaki, an immunologist at Yale University, disclosed to Live Science in an email.
What’s more, researchers should even now make sense of how the infection enters the cerebrum in any case, and whether it tends to be kept out of the mind, the creators noted in their report.
Human, mouse and little-brains
To see whether SARS-CoV-2 could break into brain cells, the study creators inspected autopsied mind tissue from three patients who died of COVID-19. They likewise directed experiments in mice infected with COVID-19 and in organoids — gatherings of cells developed in a lab dish to emulate the 3D structure of brain tissue.
“This study is the first to do an extensive analysis of SARS-CoV-2 [brain] infection using three models,” said Dr. Maria Nagel, a teacher of nervous system science and ophthalmology at the University of Colorado School of Medicine, who was not engaged with the investigation.
Already, there were just “rare case reports” of SARS-CoV-2 RNA and viral particles found in after death tissue from patients, Nagel, who represents considerable authority in neurovirology, disclosed to Live Science in an email.
In the organoids, the group found that the infection could enter neurons through the ACE2 receptor, a protein on the cell surface that the infection uses to enter the cell and trigger infection. They at that point utilized an electron microscope, which uses light emissions particles to enlighten the tissue, to look inside infected cells.
They could see Covid particles “budding” inside the cell, exhibiting that the infection had commandeered the neurons’ interior apparatus to assemble new duplicates of itself.
While settling in infected cells, the infection additionally caused metabolic changes in close by neurons, which were not infected. These close by cells ceased to exist in enormous numbers, recommending that the tainted cells may take oxygen from their neighbors so as to continue delivering new infection, the creators noted.
“We do not know if similar events are taking place in infected people,” however there is some proof they may be, Iwasaki noted. In the autopsied tissue, the group discovered SARS-CoV-2 had contaminated a few neurons in the wrinkled cerebral cortex.
Close to these tainted cells, they discovered proof of “small strokes” having occurred, indicating that the infection may take oxygen from close by cells in the mind similarly as it did in the organoids, Iwasaki said.
Notably, the infected cerebrum tissue was not overwhelmed with immune cells, as may be normal. At the point when the Zika infection or rabies infection attacks the cerebrum, an enormous number of invulnerable cells normally follow, the creators noted.
So it’s conceivable that when SARS-CoV-2 figures out how to invade the mind, it might some way or another getaway the body’s commonplace guard against such attacks.
It’s not yet known how this bizarre immune response may influence the course of the disease, however it might make the infection more hard to clear from the cerebrum.
What’s more, however barely any immune cells run to the site of infection, passing on neurons close by can trigger a chain-response in the sensory system that despite everything prompts destructive aggravation, the creators noted.
At last, in the mouse explores, the creators genetically changed one group of mice to communicate human ACE2 receptors in their cerebrums, while another group of mice just bore the receptor in their lungs.
The main arrangement of mice quickly started getting in shape and died inside six days, while the subsequent set didn’t get more fit and endure.
Furthermore, in the mice with cerebrum infection, the plan of veins in the mind changed significantly, apparently to divert supplement rich blood to “metabolically active hot spots” where the infection had assumed control over, the creators composed.
Next stages
The organoid and mouse studies offer insights at how deadly SARS-CoV-2 can be on the off chance that it arrives at the cerebrum. Yet, presently, researchers must check whether similar outcomes continue to people.
“Every experimental system has its limitation,” Iwasaki noted. For example, COVID-19 disease may advance contrastingly in mice than it does in people, and keeping in mind that organoids to some degree take after a little cerebrum, they don’t contain safe cells or veins like the full-size organ, she said.
Also, “in humans, virus is not directly introduced into the brain” for what it’s worth in mouse tests, Nagel said. Researchers should look at more autopsied tissue from COVID-19 patients to decide if the discoveries of this fundamental stir hold up in bigger gatherings of individuals.
Nonhuman primates contaminated with SARS-CoV-2 could likewise fill in as exploration models, since the flexibly of human cerebrum tissue is restricted, Nagel said.
“Virus may be present in specific brain regions or may have more indirect effects on neurological function,” Nagel included. Specifically, a few patients experience side effects suggestive of incessant exhaustion condition for quite a long time after their underlying COVID-19 disease grabs hold; it’s been recommended that the disorder emerges from changes in hormone work directed by the particular pieces of the cerebrum, she noted.
Another key inquiry is whether the “virus affects the respiratory center in the brainstem — contributing to respiratory failure in critically-ill COVID patients,” she said.
Also, researchers despite everything need to make sense of how the infection sneaks into the cerebrum in any case.
At the point when researchers discovered that COVID-19 can disturb individuals’ capacity to smell and taste, some theorized that the infection may infect the brain straightforwardly by going through nerves in the nose, Live Science recently revealed.
The infection may attack the cerebrum through the nose, Iwasaki concurred, or it may enter through the bloodstream by intersection compromised regions of the blood-brain barrier — a wall of tissue that typically isolates brain tissue from coursing blood and permits just certain substances through.